In recent years, Pilates has gained traction not just as a popular fitness trend but also as a valuable tool for rehabilitation, particularly among neurological patients. This mind-body practice, known for its emphasis on core strength, flexibility, and mindful movement, is increasingly being recognized for its therapeutic benefits.
As more healthcare professionals advocate for holistic approaches to recovery, Clinical Pilates has emerged as an effective method for enhancing mobility, improving balance, and promoting overall well-being in individuals with neurological conditions.
Let’s take a closer look at the advantages of incorporating Clinical Pilates into the rehabilitation journey for neurological patients.
1. Improved Mobility and Flexibility
One of the primary goals of rehabilitation is to enhance mobility. Clinical Pilates focuses on controlled movements and stretching, which can help improve flexibility. For neurological patients who suffer from changes in muscle tone, muscle tightness and joint stiffness, pilates exercise can result in a better range of motion in joints, making daily activities easier and more manageable.
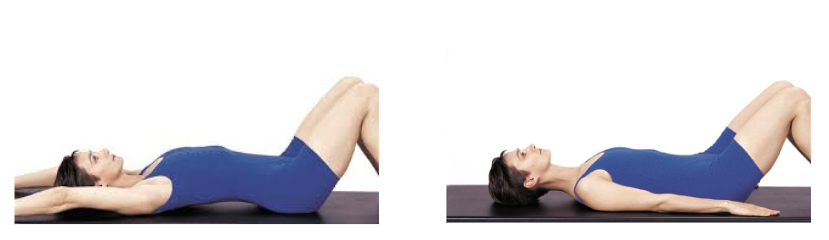
2. Strengthening Core Muscles
A strong core is crucial for maintaining balance and stability. Clinical Pilates emphasizes core strength through various exercises that target the abdominal muscles, lower back, and pelvic floor. Strengthening these areas can help neurological patients regain control over their movements and improve postural stability.
3. Enhanced Balance, Coordination and Proprioception
Many neurological conditions can affect balance, coordination and body awareness, also known as Proprioception. Pilates exercises promote this sense of body awareness and spatial orientation, helping patients develop better motor control and coordination of their movements. As balance improves, patients may experience reduced falls and an increased sense of confidence in their mobility.
4. Customized and Adaptive Approach
Clinical Pilates is highly adaptable, making it suitable for individuals with varying levels of ability. Physiotherapists are trained in working with neurological patients and can tailor exercises to meet specific needs and limitations, ensuring a safe and effective rehabilitation experience. This personalized approach encourages patient engagement and promotes steady progress.
5. Pain Management
Chronic pain can often accompany neurological conditions. Pilates emphasizes gentle movements and proper alignment, which can help alleviate discomfort. The focus on controlled breathing during exercises also promotes relaxation, reducing stress and tension that may contribute to pain.
6. Social Interaction and Support
Participating in group Pilates classes can offer social benefits as well. Engaging with others facing similar challenges fosters a sense of community and support. This social aspect can be particularly beneficial for mental well-being, reducing feelings of isolation that can accompany neurological conditions.
7. Mental Health Benefits
Physical activity, including Clinical Pilates, has been shown to improve mental health. The focus on movement, breathing, and relaxation can reduce anxiety and depression, common among individuals with neurological issues. As patients gain strength and mobility and work towards achieving their goals, their confidence often increases, positively impacting their mental outlook.
8. Promotes Functional Movement
Ultimately, the goal of rehabilitation is to restore functional movement. Clinical Pilates emphasizes movement patterns that translate to everyday activities, making it easier for patients to perform tasks like walking, sitting, and standing. This functional approach can lead to greater independence and improved quality of life.
Clinical Pilates offers a holistic approach to rehabilitation for neurological patients, addressing physical, emotional, and social aspects of recovery. By improving strength, balance, and body awareness, it empowers individuals to regain control over their movements and enhance their overall well-being. If you or a loved one is navigating a neurological condition, consider incorporating Clinical Pilates into your rehabilitation plan for a supportive and effective path to recovery.